The Vagus Nerve and Hepatic Portal Vein: Potentially a Key Step in Solving the Obesity Epidemic
Emmanuel Gitu • 2024-04-07
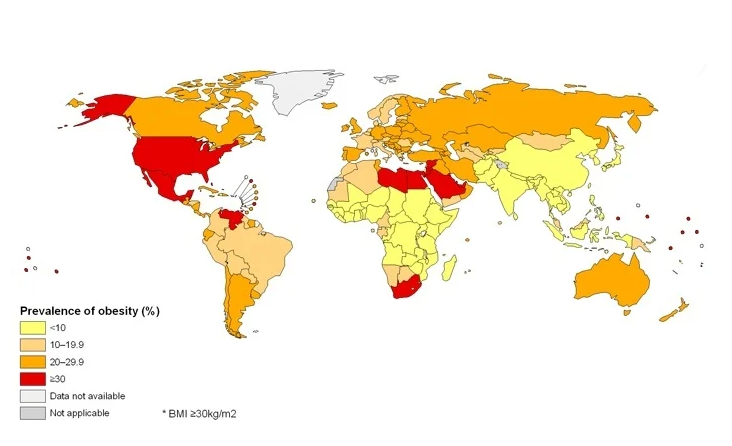
𝙄𝙣𝙨𝙩𝙞𝙩𝙪𝙩𝙚 - 𝙉𝙚𝙪𝙧𝙤𝙨𝙘𝙞𝙚𝙣𝙘𝙚 𝙃𝙖𝙧𝙫𝙖𝙧𝙙 𝙐𝙣𝙞𝙫𝙚𝙧𝙨𝙞𝙩𝙮 The obesity epidemic in primarily Western countries has often been blamed on the modern fast food diet where meals are often filled with sugars and fats for palatability.
Figure I. A map of the prevalence of obesity across the world.
Introduction:
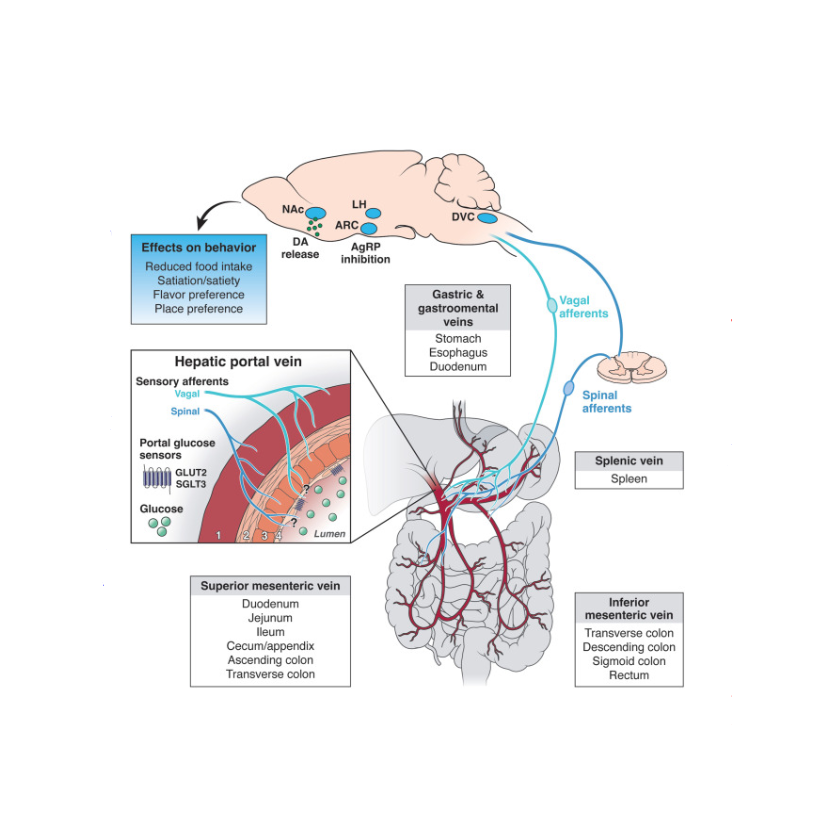
It is widely recognized that these nutrients activate reward circuitry in the brain whereby the consumption of more of that food causes a release of dopamine increasing the craving for that food and so on. Scientists have often conjectured about the specific neural circuitry behind this excessive consumption of nutrients and one nerve might be a key part of the answer. The vagus nerve is often known through articles or videos for how its stimulation may help with reducing anxiety but new research may show a link between the vagus nerve and excess consumption of sugar and fats. First, let’s start off with the biology of the bodily system researchers are focusing on. The common hepatic branch of the vagus nerve facilitates communication between the brain and digestive gastrointestinal organs such as the liver, duodenum, stomach, and pancreas (Warne et al. 2007). Afferent sensory signals are sent from the GI tract organs to the brain and efferent motor signals are sent from the brain back to the GI tract organs. Specifically in the liver the major vein that transports blood to the the liver is the hepatic portal vein, which is also innervated by the vagus nerve
Figure II. Diagram depicting putative connection between the HPC and different feeding centers of the body. Bacharach et al. 2023
Research Description:
In previous studies, a vagotomy, cutting of the vagus nerve, of the common hepatic branch of the vagus nerve has been shown to have an inhibitory effect on excessive fat, specifically lard. The logic being that this disruption of the neural circuitry halts the desire to consume more and more food. However some researchers have thought the experiment done to be too invasive with a complete vagotomy of the hepatic branch of the vagus nerve. The vagal sensory neurons play a role in many physiological functions, so doing a complete vagotomy could introduce several extraneous factors into the experiment that manipulate the results. The question of which vagal nerve connection (brain and stomach, brain and pancreas, brain and liver, etc.) is directly related to or most influences excessive consumption of nutrients is still on the table.
In other previous studies, it has been shown that low levels of glucose in the hepatic portal area trigger a metabolic response in the form of initiating a meal. It has also been shown, to a lesser degree, that infusions of glucose into the hepatic portal vein cause termination of an ongoing meal, but this has been disputed in the research community with many experimental factors playing a role in different results. However these previous studies still show conclusive evidence that the hepatic portal vein may play a role in excessive fat and sugar intake.
A 2024 study on the neural circuitry that promotes overeating found some very interesting and groundbreaking conclusions. The purpose of the study was to define the neural mechanisms for macronutrient-specific post-ingestive reinforcement of overeating (McDougle et al. 2024). Basically the question was whether there were specific neural pathways for different nutrients such as sugar and fats. Understanding this could help with medical treatment of obese individuals with eating habits pertaining to a specific nutrient, like consuming too much sugar or fats.
In this study using mice, the researchers used a novel technique to image nodose ganglion neurons, which house the soma of the neurons. Using this technique they found that different vagal subsets are activated via different stimuli. In other words, the vagal sensory neurons responded either to fat intake or sugar intake. They also found that the vagal sensory neurons are necessary for the reinforcement of overeating and that fat and sugar consumption engage different central reward circuits to cause dopamine release.
Figure III. Cages of lab mice at an unnamed institution UNOL/ISTOCK
In addition to understanding the role of vagal sensory neurons, the researchers were also able to discover the physical site of sugar and fat sensing. Their data suggests that the duodenum is a core sensing site for sugar and fat but sugar sensing also occurs at the hepatic portal vein. This reaffirms the error of a complete vagotomy in the previous study and the necessity for the current study.
Research Reflection:
These findings have profound implications for the treatment of obesity. Understanding the specific neural pathways and physical sites involved in nutrient sensing and overeating can lead to the development of targeted therapies. For instance, interventions could be designed to modulate the activity of specific subsets of vagal sensory neurons, potentially reducing the overconsumption of particular nutrients like sugars and fats.
If further research confirms the role of the vagus nerve in nutrient-specific overeating, it could be adapted to target specific branches of the vagus nerve, providing a novel and less invasive treatment option for obesity. This approach could help reduce the excessive intake of sugars and fats, thereby addressing one of the root causes of obesity.
The broader context of these findings ties into our understanding of diet and reward systems in the brain. The modern fast food diet is not just about convenience and taste; it's deeply connected to how our brains are wired to seek out high-calorie foods. This behavior likely has evolutionary roots, where consuming energy-dense foods was advantageous for survival. However, in today's environment, where such foods are abundant and easily accessible, this once-beneficial trait can lead to negative health outcomes like obesity.
The interplay between the vagus nerve and the brain's reward circuitry highlights the complexity of eating behaviors. It's not simply a matter of willpower or personal choice; biological and neural mechanisms significantly influence our eating habits. By targeting these mechanisms, medical treatments can become more effective in helping individuals manage their weight and reduce the risk of obesity-related diseases.
Personal Research Contribution:
As a researcher in this field, it was interesting as I conducted my own studies on the role of the vagus nerve in preventing the excessive consumption of sugar and fat. Specifically, I researched how vagal sensory nerve fibers influence eating patterns leading to non-alcoholic fatty liver disease, a condition primarily caused by excessive consumption of sugar and fats. Similar to McDougle’s research, I believe that hepatic portal vein (HPV)-innervating vagus sensory neurons are essential to prevent excessive eating of sugar and fat.
Using mice models we were able to target the specific vagus nerve fibers that connect the brain to the HPV and, in half the mice, chemically sever that connection. The experimental setup (see image below) divided the mice into two groups: severed vagus connection and normal vagus connection. It controlled for calories of sugar and fat and, with the 5 hour water restriction, the mice had an incentive to lick the solution as well. With this set up I was able to collect data on the intake of both sugar and fat for both mouse groups.
Personal Research Reflection:
The data I recorded from the experiments showed that there was no statistically significant difference in the number of licks of both sugar and fat solution in each group of mice. The results of the experiments were essentially inconclusive but there is still a lot to learn from the procedure.
Starting off with the experimental errors I believe there are two major ones. First off is the sample size of the mice groups. In total we used 10 mice, 5 per group, which may be too small to glean any significant results. There is also the question of whether the level of vagal nerve ablation was enough to create two independent groups. If the chemical severing of the HPV-vagus-brain connection was not complete, then that could skew the results of the experiment.
Although one might deem this experiment to be a failure, it is incredibly important to take away not only the successes, but also the mistakes of an experiment. This can help future researchers design experiments that yield more accurate results. Transparency within biomedical and neuroscience research is incredibly important as the falsification of data and results can lead to wrong information being widely accepted in the scientific community. A future Equity Journal article will discuss the negative implications of the falsification of data in biomedical research.
Conclusion:
Figure VI. Depiction of the calorie dense, high nutrient containing food often consumed in the Western world.
The recent research on the vagus nerve and its role in nutrient-specific overeating adds to our understanding of the neural mechanisms underlying obesity. By identifying the specific vagal sensory neurons involved in fat and sugar intake and their corresponding central reward circuits, scientists have opened new avenues for targeted obesity treatments. These findings underscore the complexity of eating behaviors and the need for innovative approaches to address the obesity epidemic. As the research progresses, these insights will lead to more effective treatments to help individuals achieve healthier eating habits and better overall health. We encourage this future research to be done in an ethical and transparent manner.
Citations:
Bacharach, Sam Z., et al. “Glucose sensing in the hepatic portal vein and its role in food intake and reward.” Cellular and Molecular Gastroenterology and Hepatology, vol. 16, no. 2, 2023, pp. 189–199, https://doi.org/10.1016/j.jcmgh.2023.03.012.
Gitu, N. E. (2023, August 10). How do vagal sensory nerve fibers influence eating patterns leading to Non-alcoholic Fatty Liver Disease?. [Google Slides Presentation]. MSAP Capstone Symposium, Philadelphia, PA, United States. https://docs.google.com/presentation/d/14o_cV6xDV2DLbYbeKRatIdc3g4iL_FGnf1kFSIMr4Jc/edit?usp=sharing
McDougle, Molly, et al. “Separate gut-brain circuits for fat and sugar reinforcement combine to promote overeating.” Cell Metabolism, vol. 36, no. 2, 6 Feb. 2024, https://doi.org/10.1016/j.cmet.2023.12.014.
Warne, James P., et al. “Afferent signaling through the common hepatic branch of the vagus inhibits voluntary lard intake and modifies plasma metabolite levels in rats.” The Journal of Physiology, vol. 583, no. 2, 30 Aug. 2007, pp. 455–467, https://doi.org/10.1113/jphysiol.2007.135996.
See More Posts
Copyright © 2021 Govest, Inc. All rights reserved.