Inequalities In Delivering Oral Health
Saleha Bilal • 2024-07-05
Oral health allows the mouth and the teeth to perform vital functions which include eating, drinking, and breathing. Good oral health prevents tooth decay, gum disease, tooth loss, and countless other deadly diseases.
Why does oral healthcare matter?
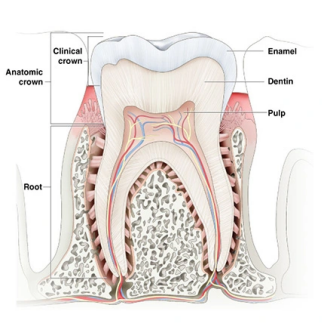
Oral health allows the mouth and the teeth to perform vital functions which include eating, drinking, and breathing. Good oral health prevents tooth decay, gum disease, tooth loss, and countless other deadly diseases. Oral health care is essential for psychological well-being as it improves the quality of life of an individual by improving their self-confidence, ability to interact with one another, and ability to perform daily functions without feeling pain or embarrassment in a social setting. Quality of life, as defined by the World Health Organisation, assesses individuals’ perceptions of their position in life in the context of the culture and value systems in which they live in relation to their goals, expectations, and concerns. The quality of life intrinsically links to the oral health care an individual receives as by being denied the standard care required to keep the mouth functioning properly, many problems arise that concern the health of an individual negatively impacting their psychological, emotional, and social well-being. Many health psychologists have identified that feelings such as optimism and resilience correlate with an individual’s quality of life, in particular how they cope with diseases. As a result, oral health symptoms such as pain in the mouth, bleeding gums, and spaces between the teeth have a detrimental effect on social well-being as oral health surveys have reported that “one in seven adults say they have low self-esteem because of their teeth”. . Moreover, the physical impact of having poor oral health care causes the structure of the teeth to be affected or altered which causes pain when biting or sensitive teeth. For example, the oral cavity is the second largest microbiota which causes 700 species of bacteria to harbour in the mouth. A range of microorganisms such as fungi, viruses, and bacteria live on the hard surfaces of the teeth as the cavity can survive on the average human body temperature. The microbes present play many critical immunological functions which include digestion of nutrition, differentiation of the host mucosa, and control of fat storage. Eventually, the accumulation of microorganisms, if not treated early, can cause the enamel of the tooth to wear away and this can lead to a small hole in the tooth which can cause infections. Also, poor oral health can lead to the tooth's structure being lost. An example of this is dental erosion which is the process affecting the enamel (which covers the atomic crown of the tooth and is made from cells called ameloblasts) and the dentin which is below the enamel and is made from cells called odontoblasts, causing these structures to wear away. Factors such as diet and environment can cause dental erosion, as a diet consisting of high levels of acidic beverages and citrus fruits can cause the enamel to become softer and lose its mineral ions such as calcium which is responsible for strengthening teeth. Also, the environment of an individual can lead to dental erosion as battery plant workers, picklers, and miners have been seen to have dental erosion as they are exposed to acidic fumes.
Inequalities in delivering oral healthcare:
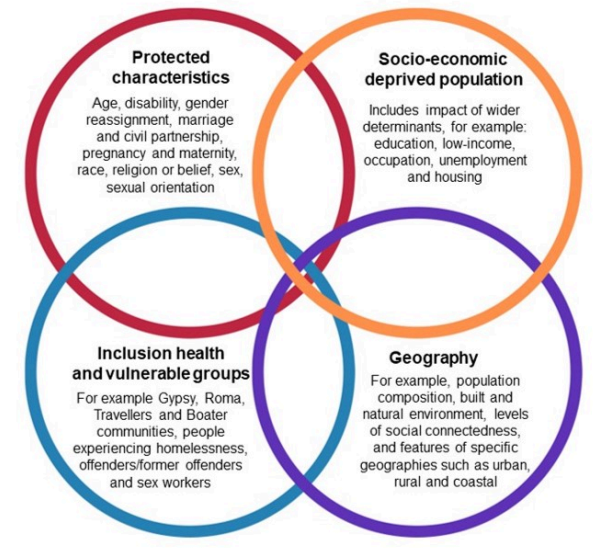
In England, oral diseases place a huge significance in terms of cost on society and the NHS as between 2017 to 2018 the NHS spent £3.6 billion on dental care for diseases which can be prevented. In this section, we will discuss the inequalities within the oral health care industry in England and Worldwide to identify the impact it is having on many communities. 1. Oral health inequalities and the socio-economic status of countries are linked as the oral health inequalities in high income countries compared to oral health inequalities in middle and low income countries (LMIC) are drastically different and to understand the impact of oral diseases it is important to acknowledge such inequalities. Researchers have identified that children from lower income groups and countries have a higher rate of tooth decay and often endure the chronic pain of dental decay, which causes them to be at a substantial disadvantage as children with poor oral health are three times more likely to miss days from school because of the pain caused which leads to a poorer school performance compared to their healthier peers. In England, almost one-fifth of children admitted to hospitals for undergoing a tooth extraction were children from the most deprived tenth of the population. Contrary to, the least deprived 10% accounted for just 4% of admissions with a primary diagnosis of dental caries.
2. Patterns of oral health inequalities have been identified in high income countries. “Researchers have observed income-related inequalities among adults in Canada, which showed more deprived groups having more decayed teeth, missing teeth and oral pain and fewer filled teeth than the more affluent"
3. Oral health inequalities in low and middle income countries is inevitable as people who lack the necessary resources are always more vulnerable to oral diseases because there is an increased exposure to risk factors and insufficient health provided. As a result, socio- economic inequality and oral health are directly linked due to extreme poverty and dental healthcare being under-resourced. It is harder to fully be aware of the socio-economic inequalities in LMICs due to a lack of coverage on the topic, compared to socio-economic in oral health being heavily reported. However, “a number socio-economic indicators have been used to measure oral health inequalities in LMICs, such as Human Development Index, urban/ rural status and GDP at the country or regional level, and income, education and occupation at the individual level.” However, we must acknowledge the fact that some of these indicators and oral health will differ between low/middle income countries and high income countries, i.e. due to geographical deprivation affecting access to adequate healthcare, the gap between urban and rural population in LMICs may be substantially larger than in high income countries.
Consequences of such inequalities:
Socio-economic inequalities and geographic deprivation has resulted in the significant increase of oral diseases due to a lack of resources and underdeveloped oral health care. Some of these infections include:
Dental Caries
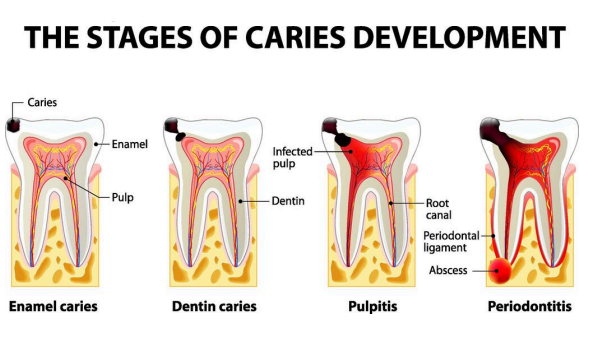
➔ Dental caries is said to be the oldest disease which is commonly found in humans. Dental caries is a chronic disease which causes the tooth structure to demineralise as a tooth adherent cariogenic bacteria which metabolises sugars to produce acid is produced.
➔ Dental caries is a huge concern for the oral healthcare industry as it is the most prevalent disease which is commonly found in low socio-economic areas. Even though dental caries can easily be prevented, due to a lack of population programmes in dental caries prevention for example affordable fluoridated toothpaste and water fluoridation, there has not been any significant improvement in the number of children and adults experiencing dental caries. Conversely, recent decades have seen an improvement in the number of children and adults experiencing dental caries in high income countries. Also, the consumption of soft drinks such as fizzy drinks and obesity in low/middle income countries contribute to the increasing diagnosis of dental caries in those countries. This puts more responsibility on a global and national level to improv the oral health of those in LMICs by raising awareness of the importance of a well maintained oral health either by providing resources or by educating the people of those areas, whilst closing the gap between and within socio-economic groups.
Periodontal diseases: ➔ Periodontal diseases such as oral cancer, orofacial deformities and orodental trauma are also common in LMICs. This is due to a lack of adequate healthcare with the combination of high rates of tobacco smoking which seems to be increasing significantly in many low income countries. Although national anti-smoking programmes work in high income countries by reducing the number of people who smoke, there is a lack of effective national programmes which target underdeveloped countries. Therefore, even though there is scarce scientific evidence on the socio-economic inequalities in oral health in low and middle income countries, there are indicators that reveal such inequalities existing as oral health shares many common risk factors with other noncommunicable diseases such as diabetes and cardiovascular diseases Conclusion: To summarise, there are a number of inequalities within oral health care which can only be overturned by raising awareness in underdeveloped countries which would reduce the gap between the high income countries and low income countries.
References: 1. Oral Health-related Quality of Life - PMC (nih.gov) 2. Oral health survey: UK adults smile less due to self-confidence issues (simplyhealth.co.uk) 3. Oral microbiome: Unveiling the fundamentals - PMC (nih.gov) 4. Divisions and Components of the Teeth - An Overview of Dental Anatomy - Dentalcare 5. What is Tooth Erosion? Causes, Diagnosis, Treatment, and Prevention (usc.edu) 6. Oral Health Inequalities - Health Action Campaign (healthactionresearch.org.uk) 7. SocialInequalities.pdf (ufl.edu) 8. Dental Caries - StatPearls - NCBI Bookshelf (nih.gov)
See More Posts
Copyright © 2021 Govest, Inc. All rights reserved.