Atherosclerosis, Thrombosis, and Ischaemia
Lennon Crandle • 2024-07-14
𝙄𝙣𝙨𝙩𝙞𝙩𝙪𝙩𝙚 - 𝙈𝙚𝙙𝙞𝙘𝙞𝙣𝙚 𝘾𝙖𝙢𝙗𝙧𝙞𝙙𝙜𝙚 𝙐𝙣𝙞𝙫𝙚𝙧𝙨𝙞𝙩𝙮
Atherosclerosis, thrombosis, and ischaemia are inter-related processes which each play a role in cardiovascular health. This essay will discuss the underpinning pathology of these processes and how they are all related.
Atherosclerosis
Atherosclerosis and its complications account for circa 50% of human deaths in the Western world. It is mostly clinically silent, until it exacerbates one’s health to the point where it causes symptoms and signs. These often occur suddenly, such as in rupture, haemorrhage, or thrombosis, which we will discuss in more detail in the next section of this essay. One of the 3 key clinical sequels of atherosclerosis is ischaemic heart disease, which can cause anigina, myocardial infarction (MI) and heart failure. Similarly, ischaemia will be discussed in great detail later in this essay. It is clear already to see there are relationships between the three processes.
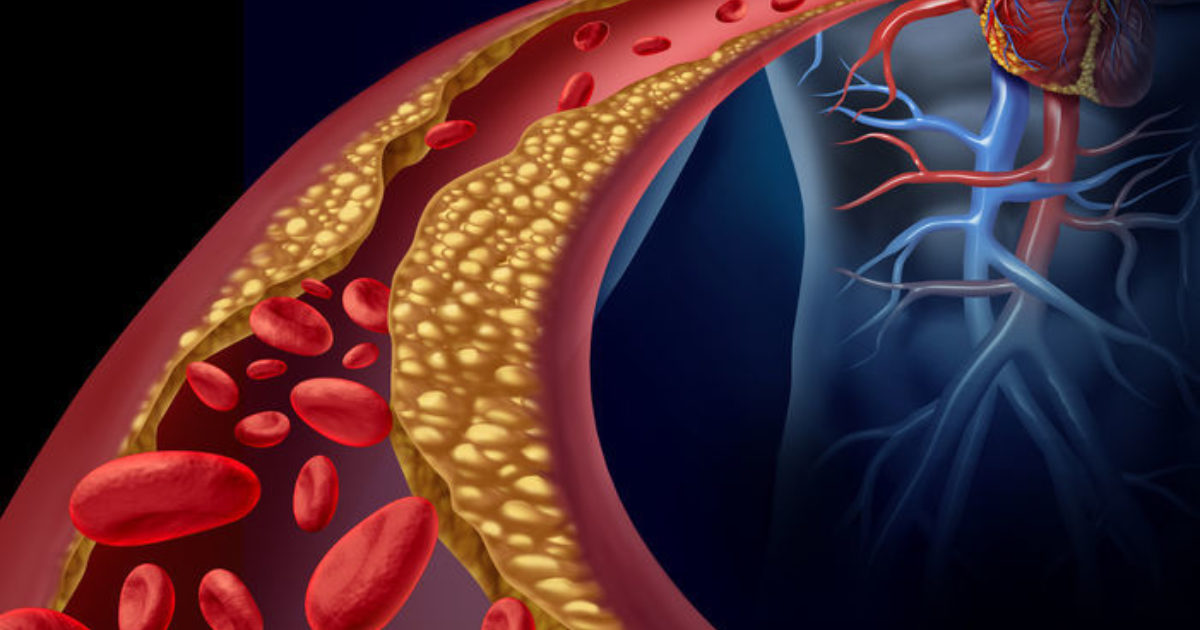
Atherosclerosis is defined as a disease of the intima of large and medium sized arteries, which is often chronic. Lesions occur, which are focal thickenings of the intima called plaques, and this causes narrowing in arteries or cardiac chambers. A key initiator of atherosclerosis is endothelial cell injury and dysfunction, leading to macrophage activation that induces multiple changes that contribute to atherogenesis (formation of fatty deposits or plaques in the arteries).
There are 2 broad classes of positive risk factors for atherosclerosis. These are the acquired (modifiable) and constitutive (non-modifiable) groups. Acquired positive risk factors include: dyslipidaemia, cigarette smoking, hypertension (both systolic and diastolic pressures are important), diabetes mellitus (|linking to dyslipidaemia, and an elevated PAI-1 levels, amongst other factors). These are all the ‘major’ risk factors. Lipoproteins are also powerful risk modifiers for atherosclerosis; dyslipoproteinaemia can increase risk. This occurs due to increasing LDL and reducing HDL levels. Entry of LDL into the arterial wall at a site of endothelial dysfunction or injury is the important early event in atherosclerotic plaque formation. Dyslipidaemia and dyslipoproteinaemia can contribute to the generation of thrombo-emboli and potentially ischaemia. In general, these risk factors can cause endothelial dysfunction and injury, the key initiating role in plaque formation, which can then lead to thrombosis and ischaemia. Constitutive positive risk factors include genetics, advancing age and male sex (due to pre-menopausal females being protected, possibly by oestrogens).
Atherosclerosis creates a vulnerable environment in blood vessels, due to plaque build-up Plaque rupture exposes the underlying tissue, triggering the coagulation cascade, leading to thrombosis. In smaller arteries, it leads to stenosis or occlusion, due to plaque progression, haemorrhage, rupture or thrombosis. This leads to localised ischaemia and as atherosclerosisprogresses, arterial lumens get narrowed more generally, causing reduced blood flow to vital organs and tissues.
Thrombosis
Thrombosis is a pathological process that occurs when the physiological mechanisms of haemostasis are activated inappropriately, forming a coagulate or blood clot. Cell injury increases thrombosis, as well as permeability, adhesion molecule and inflammatory mediator expression, macrophage and T cell entry. This is related to atherosclerosis, as previously discussed, because cell injury and inflammation (macrophages) are also implicated.
In advanced atherosclerotic lesions, platelets have a role in being involved in thrombosis secondary to plaque ulceration or rupture, this leads to thrombosis and embolisation of plaque fragments. When the plaques rupture, this exposes the underlying tissue, causing platelets to adhere to the damaged area. This initiates the formation of the thrombus, which can partially or completely block the blood vessel, which can lead to ischaemia, as discussed. So, platelets are involved in relating the two processes, and allowing atherosclerosis to progress to thrombosis. An embolism is essentially a motile thrombus. It is a blood clot that is able to move through the blood and ‘embolise’ to other regions of the organism via the blood. Cerebral artery thrombosis/embolism may cause cerebral infarction, as well as shock. MI is usually caused by coronary artery atherosclerosis, complicated by thrombosis. This can then cause mural thrombosis, occurring on the endocardium lining the infarct.
Ischaemia
This is defined as inadequate local blood supply to an organ, i.e. an insufficient quantity of blood (not an inadequate quality of blood, but this can often worsen ischaemia). Infarction, as previously mentioned, is necrosis due to ischaemia. One of the 5 causes of ischaemia is internal narrowing or occlusion of vessels, caused by atherosclerosis, thrombosis and embolism (sometimes termed thrombo-emboli). This is the primary link between the three processes.
Some consequences of ischaemia include: hypoxia, poor supply of nutrients (e.g., glucose and amino acids) and failure to remove waste products of metabolism. These changes lead to reduced aerobic and anaerobic respiration, which causes damage to cell phospholipid bilayers, mitochondria, cytoskeleton, proteins and therefore dysfunction, and influx of Ca 2+ . Loss of cell function may occur rapidly and long before morphological changes appear, e.g. myocardial cells stop contracting just 1 minute after blood supply is occluded. Ultrastructural changes take 30 minutes to occur after ischaemia, and histological changes 4-12 hours.
The outcome of ischaemia is dependent on many intuitive factors such as the degree and size of block, anatomy of organs, susceptibility/sensitivity of individual cell types to ischaemia. This is another relationship ischaemia has with atherosclerosis and thrombosis – how the extent of the latter 2 affects the outcome of ischaemia. Transient ischaemia may be caused by unstable thrombi, which commonly occurs in the brain. Ischaemia can thus be persistent in stable blockage.
Conclusion
In summary, atherosclerosis is a condition of plaque build-up and disease of the intima that sets the stage for acute events such as thrombosis, a progression which plaque rupture and platelet aggregation are both implicated in. Thrombosis, in turn, can cause ischaemia by obstructing blood vessels, as well as embolisation, which is the potential for motility of the thrombus, causing spread to other regions of the peripheral vasculature via the blood. These processes are thus interconnected and contribute to the progression of cardiovascular diseases, including heart attacks, strokes, and peripheral vascular diseases.
See More Posts
Copyright © 2021 Govest, Inc. All rights reserved.